Abstract
Introduction: allogeneic hematopoietic stem cell transplantation (alloHSCT) is a potentially curable option for patients with hematologic diseases. When considered candidates, patients face barriers to receive a transplant such as disease activity, education, financial constraints, donor availability, among others. These factors are particularly harder to overcome for patients in low- and middle-income countries. Therefore, we aimed to analyze factors that limit or favor access to an alloHSCT in a population that has been HLA typed and therefore with a potential intent-to-transplant.
Methods: we retrospectively reviewed records from 2015 until the start of the COVID19 pandemic in two of the largest Mexican government-funded transplant centers in two geographic regions in Mexico with in-house HLA typing, in one of them, an outpatient transplant strategy is followed for most patients. HLA-typed patients who were potentially eligible for transplantation were included and their outcomes were assessed in an intent-to-transplant basis. We compared the outcomes of patients who underwent transplantation to those who did not and evaluated contributing barriers to access alloHSCT with multivariate logistic regression. This study was performed on behalf of the TCTMX working group.
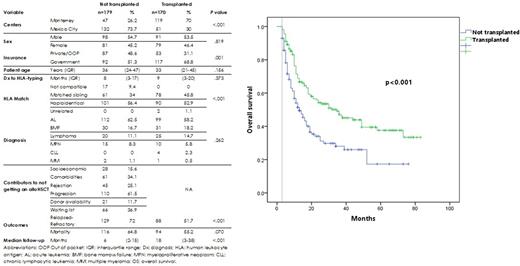
Results: we screened 391 patients, 42 were excluded as they had no indication for alloHSCT with a total of n=349 patients analyzed. The median age at HLA-typing was 34 years (IQR 22-46); n=211 (60.5%) had acute leukemia (AL), n=61 (17.5%) bone marrow failure (BMF), n=45 (12.9%) lymphoma, n=25 (7.2%) myeloproliferative neoplasms (MPN), n=4 (1.1%) chronic lymphocytic leukemia (CLL) and n=3 (0.9%) multiple myeloma (MM). Most patients (n=209, 59.9%) had government insurance coverage. Median time from diagnosis to HLA-typing was 8 months (IQR 3-19). The majority had a potential donor (95.1%): n=191 haploidentical (54.7%), n=139 a matched sibling donor (39.8%) and 2 an unrelated donor (0.6%). Almost half of them eventually received a transplant (n=170, 48.7%), the median time to HLA-typing to alloHSCT was 3 months (IQR 1-6). Sex, age and diagnoses were similar between transplanted and non-transplanted patients, while non-transplanted patients had a higher proportion of not compatible and haploidentical donors. Disease activity or progression was the biggest barrier for transplantation, followed by waiting for a hospital bed and comorbidities (Table 1). Donor availability limited transplant access for only 11.7% of patients. Access to transplantation was favored by private/out-of-pocket payment (OR 2.1 95% CI 1.3-3.4), and receiving care in the outpatient center (OR 6.4 95% CI 4-10.5), while HLA matching was not (OR 1.1 95% CI 0.8-1.7). Non-relapse mortality (NRM) in alloHSCT was 22.3%. Median overall survival (OS) from the intent-to-transplant cohort was 15 months (CI 95% 11.4-18.5). An OS landmark analysis for patients alive at or beyond 3 months (the median time from HLA-typing to alloHSCT) showed prolonged survival in alloHSCT (35 vs 13 months, p <.001), figure 1. By the time of the analysis 139 patients (39.8%) were still alive and 132 (37.8%) were event-free.
Conclusion: the most frequent barrier to transplantation was the disease itself, followed by the transplant waiting list and comorbidities. Access to out-of-pocket resources and an outpatient strategy or center effect favored alloHSCT. In the era of haploidentical transplantation, donor availability was a smaller issue. An approach to overcome barriers could be to implement outpatient transplantation and eliminate the waiting list barrier without increasing NRM, to improve the health policy in the direction of more patients get coverage, patient education to diminish the rates of rejection and improve their comorbidities. To our knowledge, this is the largest intent-to-transplant analysis in a population that has been HLA-typed.
Disclosures
Gomez-Almaguer:BMS: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Janssen: Consultancy, Honoraria. Gomez-De Leon:AbbVie: Honoraria, Other: advisory board.
Author notes
Asterisk with author names denotes non-ASH members.